- Risk factors for developing dental implant infection include poor oral hygiene, smoking, and previous periodontal disease.
- Symptoms of dental implant infection include swelling, changes in gum color, bleeding, and a loose implant. You may also develop fever, ear throbbing, and pain that does not go away even with medication.
- Dental implant infection is treatable at early stages. Treatment methods include mechanical cleaning and surgical procedures.
Smile like never before, starting today. Use Authority Dental to book dental implant dentists near you. It's simple, fast and reliable.
Do you suspect you may have a dental implant infection? Here's everything you need to know.
Risk factors for dental implant infection

Picture by Authority Dental under CC 2.0 license
The most common causes of implant infection are:
poor oral hygiene,
smoking, and
previous periodontal disease.
Proper implant aftercare is vital. If you do not brush and floss daily, you allow bacteria and fungus to enter and colonize your mouth. These gradually migrate towards the soft and hard tissues surrounding the implant. Infections may lead to a variety of dental implant problems.
Tobacco users have a higher concentration of the enzyme arginase in their saliva. It is argued that it lowers nitric oxide production. This makes saliva more acidic, creating a perfect environment for bacteria to thrive. Smokers are therefore more vulnerable to dental implant infections.
Patients with a history of periodontitis are also at higher risk. It certainly has to be treated before implantation can take place, but gum disease has a tendency to come back. Bone loss is likewise more prominent in such cases, leading to a larger rate of implant failure.
All in all, implant infection is almost always associated with patient-related risk factors. The following are worth noting, but the rate of infection caused by these is very low:
Dental implants infection symptoms
If you observe any of these signs, immediately contact your dentist:
swelling around the implant,
changes in the color of the gums,
bleeding from the implant site,
a fever,
throbbing in your ear, and
pain that does not respond to medication.
Harry Lee, DMD, explains: "One of the most significant insights from practice is that this disease is almost always silent at first. Patients do not feel pain, so they ignore the subtle bleeding or swelling—the key early warning signs, much like early gum disease."
"I warn patients that if they notice the gum color changing to a deep red or purple, or if they can feel the implant area weeping or bleeding when they brush, they need to call immediately," he stresses.
Soreness is relatively rare with implant infection, but if it is present, it usually indicates a severe problem. Other causes for concern are similar to those of sinus lift and bone graft infection.
If you experience any of these symptoms, search for emergency dental care near you immediately.

Dental implant infection symptoms also include a deep probing depth of the peri-implant pockets and gradual bone loss in the affected area. Those, however, can only be diagnosed by a professional such as a dentist or periodontist.
Stages of dental implant infection
Tooth implant infection can be described in two stages. The first is called peri-implant mucositis. When left untreated, it can transform into a more serious condition, peri-implantitis.
Both progress similarly to gum disease but may develop more rapidly. This is because the attachment of an implant is less durable than that of a natural tooth. Signs can even occur years after implant placement.
Peri-implant mucositis
Patients may experience soft-tissue inflammation around the implant. When no bone loss is detectable, the infection is entirely reversible. This does not, however, mean that the condition is not serious.
In more severe cases, surgical treatment might be necessary. One way or another, peri-implant mucositis should be dealt with as soon as possible to prevent further damage. If left unattended, it could lead to the implant's future loss.
Peri-implantitis
The second stage of dental implant infection is called peri-implantitis. It affects the soft and hard tissues around the rod and is accompanied by bone loss in that area. This condition occurs after osseointegration, when the restoration (for example, a crown) is already in place.
Peri-implantitis does not inevitably lead to implant failure. It can and should be treated as soon as symptoms become apparent.

How to treat a dental implant infection
First, an X-ray will be performed to determine whether there is any bone loss. This is followed by periodontal probing. This allows for an accurate diagnosis of the infection stage. Then, the dentist will suggest a treatment plan.
The following are the most popular remedies. Usually, a combination is performed.
Mechanical cleaning
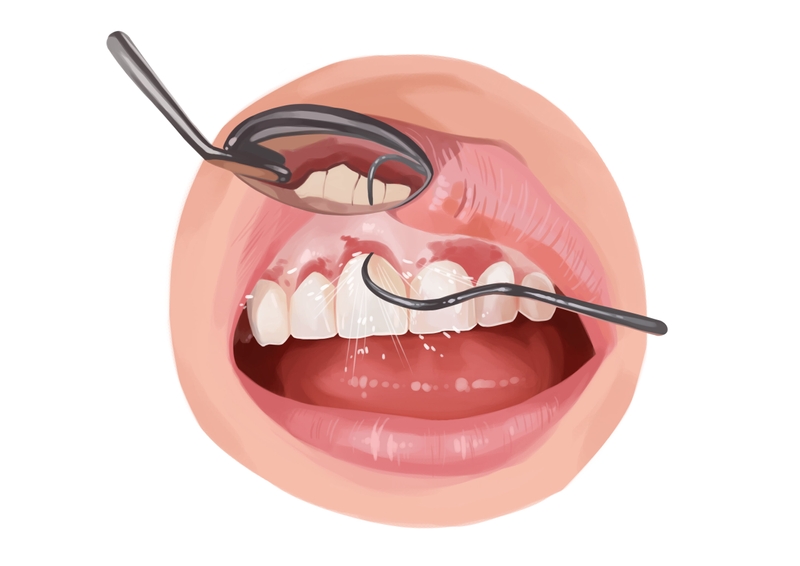
Picture by Authority Dental under CC 2.0 license
Shallow mucosal pockets can be cleaned with an ultrasonic device or carbon fiber curettes. This is called sub-mucosal debridement. High-frequency waves allow the dentist to remove contaminated material around the implant.
If the mucosal pockets are 5mm or deeper, your dentist might suggest polishing with a rubber cup and paste, mechanical flossing, or delicate scaling instruments. In such a case, the instruments have to go deeper, and it is important not to roughen the rod's surface.
Mechanical debridement is often conducted in conjunction with locally administered antiseptics. This is done only if the pocket depth is greater than 4mm.
Surgical procedure
Surgical management of implant infection is generally performed when the rod is placed in a non-aesthetic site.
The gums are cut open and flapped back to allow better access to the contaminated area. A mechanical cleaning is performed, often in conjunction with antiseptics. This procedure is sometimes referred to as open-flap debridement.
This option comes with many potential complications. The exposure of porous membranes can lead to further infection, especially during the healing period. It should be performed only if other forms of treatment fail.
Dental implant infection antibiotics

Picture by Authority Dental under CC 2.0 license
The dentist will examine the periodontal condition of the remaining teeth. Based on this information, he or she will determine whether to administer antibiotics locally or systemically.
If peri-implantitis is limited to the immediate vicinity of the implant and no other disease is present in the mouth, localized antibiotics might be prescribed. They will be distributed to the affected site for a few days.
If the infection spreads to a larger area of the mouth, antibiotics may be administered systemically. The same happens when the patient is simultaneously suffering from periodontitis.
Antibiotic treatment may have to be repeated within a few weeks or months.
Implant removal
If peri-implant mucositis has progressed to peri-implantitis and significant bone loss has occurred, the implant may need to be removed. This can be done with a surgical instrument called a trephine.
Alternatively, the dentist might decide to allow bone loss to continue until the implant can be extracted with forceps. This decision is made when there is less than 3-4 mm of supporting bone.
Some patients may qualify for reimplantation after bone grafting and several months of healing.
FAQ
Can an infected dental implant be saved?
Often, yes. If the infection is diagnosed quickly and treatment begins soon after symptoms appear, the implant can be saved.
It should be a straightforward process if there were no bone loss. The most common treatment is a mechanical cleaning. You will likely get antibiotics and might have to undergo surgery.
Who treats dental implant infection?
A periodontist may have to treat your infection, especially if it is severe. Contacting your primary dentist, however, is always a good place to start.
Can I get dental implant infection years after surgery?
Yes. Peri-implantitis leads to late implant failure. This means it happens after the restoration, such as a crown or retained denture, is already in place. Infections are usually caused by smoking or poor oral hygiene, and rarely happen immediately after surgery.
What happens if you don’t treat infection?
Infections in the mouth can proliferate. Peri-implantitis develops much faster than gum disease. It can lead to bone loss and implant failure. It is not uncommon for neighbouring teeth to suffer as well.
What is more, an abscess could form and transfer bacteria into your bloodstream. If that happens, you are looking at a serious, life-threatening situation.
How to prevent dental implant infection?
The best way to prevent infection is to quit smoking and practice excellent oral hygiene. This means brushing after every meal and flossing at least once a day. Remember to visit the dentist for regular check-ups, too. The dentist will perform routine X-rays and implant maintenance during these visits to detect problems early. Implants cannot get cavities, but that does not mean they do not require care.
References
- Smoking increases salivary arginase activity in patients with dental implants
- Effect of periodontitis history on implant success: a long-term evaluation during supportive periodontal therapy in a university setting
- Management of peri-implantitis
- Peri-Implant Bone Loss and Peri-Implantitis: A Report of Three Cases and Review of the Literature
- Peri-implant mucositis
- Peri-Implantitis
- Comparative biology of chronic and aggressive periodontitis vs. peri-implantitis
- Peri-implant health, peri-implant mucositis, and peri-implantitis: Case definitions and diagnostic considerations
- Peri-implant mucositis
- Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions
- Osseointegration
- Non-surgical therapy for the management of peri-implantitis: a systematic review
- Adjunctive Systemic and Local Antimicrobial Therapy in the Surgical Treatment of Peri-implantitis: A Randomized Controlled Clinical Trial
Harry Lee, DMD
The conversation around dental implant infection, or peri-implantitis, is one of the most critical I have with my patients. I emphasize that while the titanium implant is nearly indestructible, the gum tissue and bone supporting it are absolutely not. I tell them to think of the implant like a high-end fence post: the post itself is fine, but if you let the dirt and debris pile up around the base, the foundation (the bone) will erode, and eventually, the post will wiggle.