- Gum disease (also called periodontal disease) is an inflammatory condition that begins as gingivitis and can progress into periodontitis. It first affects the gums and, if left untreated, can damage the supporting bone and lead to tooth loss.
- Symptoms of gum disease include bleeding, inflammation, and receding gums. It can also lead to bad breath, sensitivity, painful chewing, and deep pockets around the teeth.
- Plaque and tartar, which form due to poor oral hygiene, are the main causes of gum disease. Treatment requires deep cleaning, scaling, and root planing, antibiotics, and, in extreme cases, surgery.
Need emergency treatment for a gum disease? Find urgent care dental near you with Authority Dental.
Do you have any signs of gum disease? Here's everything you need to know.
Gingivitis vs. periodontitis
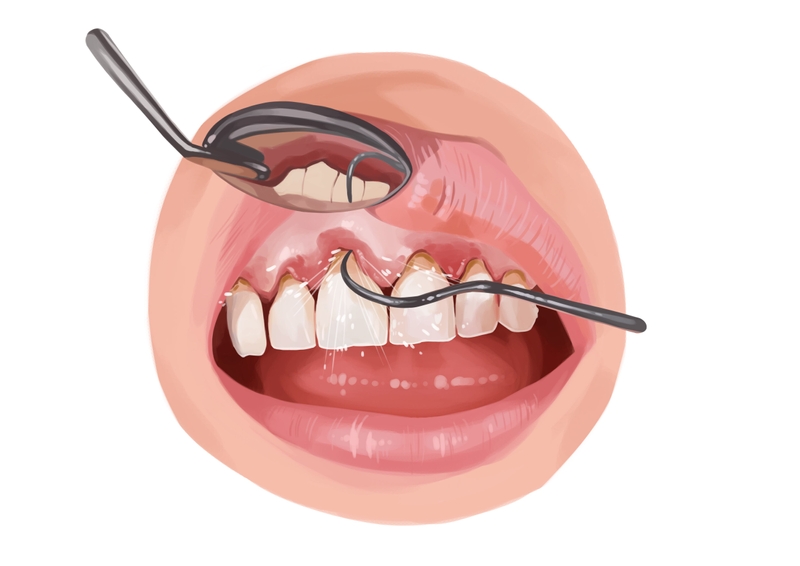
Picture by Authority Dental under CC 2.0 license
Gingivitis and periodontitis are 2 stages of gum disease.
Gingivitis is the initial stage of gum disease and acts as a warning sign. Gums around the teeth are inflamed. Once this travels below the gumline into the bone, the gingiva starts to shrink and recede away from the teeth. The surrounding structures are likely to get damaged.
Periodontitis occurs when gum pockets are deeper than 4mm. When the attachment between gums and teeth begins to break down, periodontal pockets form. There, bacteria set up a habitat and multiply, causing significant inflammation. Once formed, these pockets are very hard to clean. It often has to be done professionally and with antibiotics.
Despite apparent differences in symptom severity, patients find it difficult to assess their gum disease stage independently. It is best to see a dental professional who will perform an exam and measure the depth of the pockets. If you notice disturbing signs, do not delay the visit, as this could allow the disease to develop.
Gum disease symptoms
The most common signs of gum disease include:
bleeding gums, especially after brushing or flossing,
red, swollen, tender, and receding gingiva,
persistent foul taste,
sensitivity to hot and cold temperatures,
painful chewing,
presence of pus in the mouth,
deep pockets around the teeth,
loose dentition, and
changes in the bite.
You will have bad breath because the bacteria in your mouth release toxins. However, this is only apparent with gum disease. Your breath should stay about the same if you only have gingivitis.
When you have receding gums, your teeth will appear longer. This happens due to tissue loss. What is more, teeth then start to shift and move as they have less support from the bone.
Sensitivity is also associated with gum recession. The sensitive parts of the teeth (not covered by enamel) become exposed. The disease will attack these more vulnerable parts of your dentition.
These periodontitis symptoms might only affect some teeth, for example, molars. That makes them harder to spot.
Sometimes there are no symptoms of gum disease, yet the problem persists. Even at advanced stages, you do not get much of a warning. That is why regular dentist visits are so important.
What causes gum disease?

Picture by Authority Dental under CC 2.0 license
The biggest culprit here is plaque and tartar buildup. This is usually the result of poor oral hygiene, including a lack of brushing, flossing, and regular dental cleanings.
Some patients may be more susceptible to the disease, however. This is linked to several factors that can make teeth and gums sensitive, leading to a quicker, increasingly aggressive progression.
Hormonal changes
These often occur during pregnancy, menopause, and menstruation. Puberty is also a dangerous time for mouth and gum health, as gum disease incidence rates are much higher for 15-18-year-olds.
Certain illnesses
Periodontitis-causing illnesses primarily target the immune system. They include cancer, HIV, and diabetes. Treatment for those who have periodontitis can make it even more of a risk.
Some medications
Spit is an important part of disinfecting and protecting the teeth, gums, and mouth. Many medications reduce saliva flow. The most prominent among them are anticonvulsant, anti-angina, antihistamine, and antidepressant drugs. You may even develop a condition called dry mouth.
In addition to proper brushing and regular dental care, some individuals explore daily oral health supplements designed to support a healthy oral microbiome. Oral probiotics are formulated to support balanced oral bacterial communities, which may contribute to overall gum health and fresh breath. These products are not a replacement for professional dental treatment and should be used alongside a comprehensive oral hygiene routine.
Lifestyle
Poor lifestyle choices such as smoking, alcohol abuse, and high stress levels also contribute to periodontitis. Dip gum disease, caused by chewing tobacco, is arguably the most direct of periodontitis-causing factors. Habits like mouth breathing also make it easier for bacteria to enter the gum cavity.
Family history of the disease
Family history and prior episodes can make you more susceptible to developing gum disease again. Many dentists refer to chronic periodontitis treatment as “maintenance” because it tends to come back.
Crooked or overlapping dentition
Orthodontic problems can make teeth harder to clean properly. Plaque loves to take up habitat in those nooks and crannies that your toothbrush cannot reach. If you find that this is true in your case, visit an orthodontist.
Poor nutrition
In addition, watch your diet for high-sugar and high-carbohydrate content—those substances like to simmer in the mouth long after the meal is gone. Deficiencies in Vitamins C and D also slow healing.
Gum disease treatment
As soon as you are diagnosed with gum disease, it is best to take action immediately to minimize its consequences. Still, there is no magic cure for periodontitis; it is rather a process.
Periodontitis remedies from home
Since periodontitis often results from poor oral hygiene, proper brushing and flossing are key. If your gums and teeth are tender, use a soft-bristle brush and go easy on your mouth. Invest in an antiseptic mouthwash to reduce bacterial levels as well. You can use hydrogen peroxide as a rinse as well.
Tobacco makes it much harder for your mouth to fight bacteria. Dip and cigarettes are an absolute no-no once you start treatment. Some dentists may even refuse to work with you until you target this issue.
A well-balanced diet can boost your body’s ability to fight off infection. Antioxidants, like those found in vegetable oils, nuts, and greens, can help repair damaged tissue.
Moreover, when your teeth start to feel loose or shift, grinding and clenching can make the problem worse. The teeth may even fall out.

Professional gum disease treatment
Whatever the stage, we recommend a checkup with your dentist, or better yet, a periodontist. He or she will conduct an exam to look for the following signs of gum disease:
pocket depth,
bleeding and swelling of the gums,
tooth movement and sensitivity, and
bone structure quality.
The last step will be done with X-rays. If the dentist concludes that you are in fact suffering from gum disease, he or she will perform a deep cleaning, otherwise referred to as scaling and root planing.
Deep cleaning occurs both above and below the gumline. Scaling involves scraping off tartar deposits. Root planing is the polishing and smoothing of exposed roots. You might get time-release antibiotics and have to return after a few weeks.
If your gums suffered significant damage, you may need a gingivoplasty for periodontitis. It is a surgical reshaping of gum tissue lost due to the disease.

FAQ
Does gum disease go away when teeth are removed?
Is Alzheimer's gum disease a thing?
Recent research shows that gum disease and Alzheimer's are linked. The bacteria that appear on the periodontium can also cause or be partly responsible for several types of dementia.
How to prevent gum disease?
Proper plaque control is key. Gum disease can be managed and even reversed this way. This means brushing after every meal, flossing every day, and coming in for a professional cleaning at least twice a year.
Antibacterial mouthwashes are great at reaching places you miss during your oral routine. Soft areas like your gums may be too sensitive for brushing, so managing bacterial growth with rinses is important.
How long does it take for gingivitis to turn into periodontitis?
If you are not in the risk group, this progression can take many months. This is good news, since the worst can be prevented. If you are keeping up with your bi-yearly appointments, your dentist will be able to diagnose the problem in time.
References
- Effects of scaling and root planing on clinical parameters and bacterial flora in periodontal pockets
- What is the difference between plaque and calculus?
- Aggressive periodontitis: case definition and diagnostic criteria
- Differences in periodontal disease-associated microorganisms of subgingival plaque in prepubertal, pubertal and postpubertal children
- The role of immune system in the development of periodontal disease: a brief review
- Salivary flow rate and periodontal infection - a study among subjects aged 75 years or older
- The Relationship between Vitamin C and Periodontal Diseases: A Systematic Review
- Evaluation of the effect of hydrogen peroxide as a mouthwash in comparison with chlorhexidine in chronic periodontitis patients: A clinical study
Harry Lee, DMD
I often call gum disease the "silent thief" of adult smiles. The biggest hurdle I face in my practice is the myth that bleeding gums are "normal" during vigorous brushing. They are not; it is a primary alarm bell. CDC data shows nearly half of Americans over 30 have some form of periodontal disease, but because it rarely hurts in the early stages, it is dangerously easy to ignore.