- Tooth decay, also known as dental caries, occurs when plaque bacteria produce acids that attack and break down the hard tissues of the teeth. Poor oral hygiene and diets high in simple sugars can accelerate this process.
- Root decay is common among patients with receding gums and the elderly.
- The type of treatment a dentist will use depends on the severity of the tooth decay. Fluoridation, fillings or crowns, and abscess intervention are just some of the possible treatments.
Need urgent dental care? Use Authority Dental to quickly connect with emergency dental clinics in your city.
Learn what tooth decay is, what causes it, early symptoms, and how it’s treated. Dentist-reviewed guide with prevention tips.
What causes tooth decay?

Picture by Authority Dental under CC 2.0 license
Tooth decay is a gradual process rather than a single event. Simply put, food particles left on the teeth can be broken down by oral bacteria, producing acids that weaken tooth enamel over time. This process is more likely to occur when proper oral hygiene is neglected, including regular brushing, flossing, and professional cleanings, especially in an oral environment that favors bacterial growth.
Along with consistent brushing, flossing, and routine dental visits, some people choose daily oral health supplements to help support overall oral balance. Oral probiotics are designed to promote a balanced oral microbiome, which may help support a healthier oral environment when used as part of good oral hygiene habits.
Risk factors of dental caries include:
a diet rich in carbohydrates and acids,
conditions that inhibit the production of saliva,
certain medications, and
some oral conditions.
Disorders such as diabetes mellitus and Sjögren’s syndrome may lead to decreased saliva flow. This substance helps thin and wash away bacteria between brushing sessions. Some medications, especially antihistamines and antidepressants, may also make this worse.
Other issues, such as receding gums and periodontitis, may also increase the risk of decay.
Types of dental caries
Dental caries are classified by location.
Pit and fissure and occlusal caries
Pit and fissure and occlusal caries are generally the same. The latter refers to the biting surface of the posterior teeth. Pits and fissures are found on this surface, with some extension to the cheek and tongue sides.
Decay on smooth surfaces of dentition is usually easy to spot and quick to diagnose. Molar teeth are likely to be affected, as they are in the back and harder to brush appropriately. This is why flossing is vital.
A good preventive method is dental sealants. A thin coating is applied to those nooks and crannies to prevent food from getting stuck—the coating bonds to the teeth.

Root caries
If decay happens below the gumline, it is considered root decay. This is a dangerous type of cavity because it occurs in the cementum. This is softer, thinner, and more vulnerable than enamel.
Decay can reach the pulp sooner than if the cavity had started in the enamel. Root caries are common among patients with receding gums and in the elderly. They develop twice as fast as cavities in other areas of the tooth.
Harry Lee, DMD reports: "I am currently seeing a significant spike in root decay, especially among older adults. Once gums recede, the exposed root surfaces—covered in thin cementum rather than tough enamel—decay twice as fast."
"I also frequently discuss the "dry mouth" factor," he adds, explaining, "many common prescriptions for blood pressure or anxiety dry out the mouth, stripping away saliva, which is our natural acid buffer. Without that constant rinsing action, bacteria thrive, turning a healthy mouth into a high-risk environment in just a few months."
Tooth decay stages
Knowing how tooth decay develops can help you adjust home remedies and prepare for your dental visit.
Initial demineralization
The first stage of tooth decay is demineralization of the enamel. This is the outer shell of the tooth, a tough substance composed of various minerals. Acids produced by bacteria dissolve the tooth structure, which shows up as chalky white spots on the teeth.
Enamel decay
If the acids and bacteria are not removed, and the teeth are not remineralized, decay of the enamel begins. This looks like darker, brown spots. These can quickly turn into lesions requiring a filling.
Up until this point, the process is reversible. If the patient neglects to address the issue, however, tooth structure can be lost. Moreover, it cannot be recovered without a dentist's intervention. The affected area may turn soft to the touch.
Dentin decay
Dentin lies directly beneath the enamel and is much softer. Decay occurs much more rapidly at this stage. What is more, dentin has tubes that connect to the tooth nerves.
Patients may experience sensitivity, especially to hot, cold, and sweet foods and drinks. Bad breath and a foul taste in the mouth are also common.
Pulp damage and death
The innermost layer of the tooth has nerves and blood vessels. If this tissue becomes irritated, it starts to swell. Cracks and fractures may appear as the tooth structure becomes undermined. This is also often painful.
If the pulp tissue dies, the tooth will stop being sensitive to stimuli, but may be tender when pressed. Pain to chewing may develop, as well as swelling in the gums and even on the face.

Can you reverse tooth decay?

Picture by Authority Dental under CC 2.0 license
If the dentin has not yet been damaged, decay can be reversed. There are some home remedies you can try, but a dental visit with a professional is always recommended. You may not be able to assess or diagnose the issue yourself.
While waiting for your appointment, you can:
incorporate fluoride and vitamin D in your diet,
consider buying toothpaste with fluoride,
chew sugar-free gum, and
Try oil-pulling.
Products containing fluoride help remineralize your teeth. It is present in some tap water across the US. Further demineralization can be prevented by chewing sugar-free gum. Most brands use xylitol, which can stimulate saliva production, neutralize the mouth’s pH, and help kill some bacteria.
Vitamin D is an important factor in maintaining your teeth's health. You can find it in foods like milk and yogurt as well as in your garden.
Sesame or coconut oil can be used to clean your mouth. Swish it around in your mouth for about 20 minutes, then spit it out. It may be a good idea to brush your teeth afterwards anyway. This is a home remedy, not a professional recommendation.
Tooth decay treatment
The type of treatment your dentist chooses depends on how severe your tooth decay is. He or she will begin with an exam to diagnose the problem and stage of the caries. Talk about any pain or sensitivity you have experienced. There might also be some X-rays and a probing session.
Fluoridation
If your tooth decay has not gotten past chalky white spots, fluoridation may be enough. Fluoride varnish will be applied to the affected teeth. This is totally non-invasive, and you will not need any anesthesia.
The dentist may also apply fissure sealants to your molars to help prevent future decay. You might receive a prescription for fluoridated toothpaste and mouthwash to use at home.
Fillings or crowns

Picture by Authority Dental under CC 2.0 license
If the tooth structure has been lost, you will need a filling. The damaged area will be drilled away under a local anesthetic to numb any discomfort. Then, either composite resin or amalgam will be used to fill the hole and build up the tooth.
When decay has eaten away at a large part of the tooth, you may need a crown. Some healthy structures may also have to be removed to accommodate it. A porcelain “cap” will restore your smile’s appearance.
Abscess intervention
If an abscess has formed, it will need to be professionally removed. Please do not attempt to burst it yourself, as the infection might travel towards the inside of your body.
The dentist will cut and release the liquid. This relieves pain significantly. The area will then be cleaned with saline solution. A root canal procedure may be necessary. In cases where the patient’s immune system is weakened or the infection has spread widely, an antibiotic is prescribed.
Root canal treatment
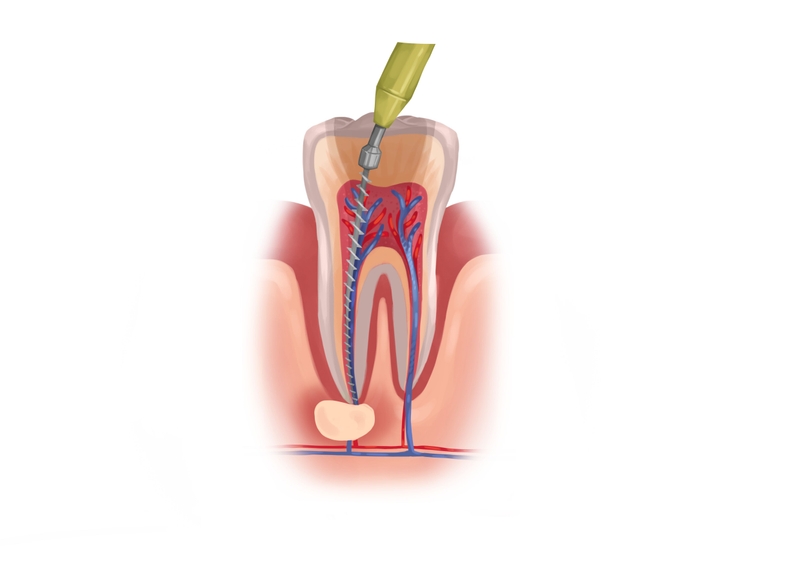
Picture by Authority Dental under CC 2.0 license
If the dental pulp is infected, you will likely need endodontic treatment. This means drilling a hole through the top of your tooth and removing all damaged matter from the inside. It may take several visits, and you might need antibiotics. Root canal treatment often ends with a large filling or a crown.
Extraction
Sometimes the damage is so severe that the tooth has to be removed to prevent further infection of the rest of your dentition and your body. Your dentist will discuss restoration options such as dental bridges and implants with you. Not replacing a pulled tooth could cause your other dentition to shift and your face to appear to sag due to a loss of support.
FAQ
How does plaque lead to tooth decay?
Plaque feeds bacteria that are naturally present in your mouth. While they digest it, they also produce harmful acids that demineralize and dissolve your teeth. The result is decay.
What are the most common tooth decay symptoms?
Can you remove tooth decay yourself?
If it has not reached the dentin, you may be able to reverse the decay at home. Fluoride and proper oral hygiene are key.
How can you stop tooth decay?
If you notice white spots on your teeth, make sure you drink fluoridated water and switch to a toothpaste that contains this mineral. Avoid acidic and sugary beverages. Even sugar-free ones with acids can erode enamel.
Make an appointment with your dentist to check out whether everything is okay. Drilling and filling may be unnecessary if you act quickly.
What if you don’t treat dental cavities?
Such neglect can lead to an abscess forming. This happens at the stage when the decay attacks the pulp. The gums become inflamed, and a pus pocket forms near the tooth.
This is urgent. The tooth may be lost, and the disease can spread via the bloodstream to the rest of the body. It puts the patients at risk of sepsis.
Can a badly decayed tooth be saved?
It all depends on your particular situation. A filling may be enough. More severe cases need root canal treatment, which may end with a crown. If the tooth structure has been completely undermined, the tooth may have to be removed.
How to prevent tooth decay?
Prevention begins at home. Brush after every meal and use floss and mouthwash once a day. Try not to eat sugary snacks high in carbohydrates, especially when you are out and have no way to clean your teeth. Any snacking should be avoided, as it raises the pH of your mouth for about 30 minutes.
Make sure to stay up to date with regular dental check-ups and cleanings. Incorporate fluoride into your diet and homecare routine to keep your teeth mineralized.
References
- The relationship between oral health and diabetes mellitus
- Sjögren Disease
- Salivary Secretory Disorders, Inducing Drugs, and Clinical Management
- Pit and fissure sealants for preventing dental decay in permanent teeth
- Interventions for managing root caries
- Demineralization–remineralization dynamics in teeth and bone
- Community Water Fluoridation
Harry Lee, DMD
In my practice, I often describe tooth decay to patients as a "slow-motion chemistry experiment." It is not just a hole that appears overnight; it is a constant tug-of-war between demineralization and remineralization. Most people are shocked when I find a cavity during a routine exam because they "do not feel anything." That is the catch: by the time you feel that sharp zing from a cold drink, the decay has usually already tunneled through the hard enamel into the softer, sensitive dentin. Statistics consistently show that caries remain the most prevalent chronic disease globally, yet they are almost entirely avoidable.